What is Osteoarthritis?
Sometimes called degenerative joint disease or degenerative arthritis, osteoarthritis (OA) is the most common chronic condition of the joints, affecting approximately 27 million Americans. OA can affect any joint, but it occurs most often in knees, hips, lower back and neck, small joints of the fingers and the bases of the thumb and big toe.
In normal joints, a firm, rubbery material called cartilage covers the end of each bone. Cartilage provides a smooth, gliding surface for joint motion and acts as a cushion between the bones. In OA, the cartilage breaks down, causing pain, swelling and problems moving the joint. As OA worsens over time, bones may break down and develop growths called spurs. Bits of bone or cartilage may chip off and float around in the joint. In the body, an inflammatory process occurs and cytokines (proteins) and enzymes develop that further damage the cartilage. In the final stages of OA, the cartilage wears away and bone rubs against bone leading to joint damage and more pain.
Symptoms of Osteoarthritis
Joints in the body are protected by cartilage. Over time, this cartilage breaks down and is ultimately lost. Bones that were once separated and cushioned by the cartilage eventually rub against each other, resulting in joint pain and damaged tissue and bone.
Joints affected most often are the spine, hips, knees, fingers, and toes. Disabling symptoms of osteoarthritis include:
- chronic pain
- muscle spasms
- stiffness and loss of motion of the joint
- synovitis (swelling caused by fluid in or near the joint)
- enlargement of joints, such as bony knobs on finger joints
- crepitus (painful grinding and joint cracking with movement)
Tissue and bone damage caused by osteoarthritis is irreversible. Osteoarthritis is managed by a wide range of medications, including NSAIDS, corticosteroids, and narcotics.
Those affected by osteoarthritis often suffer from side effects of these medications. Joint replacement and other forms of surgery may be necessary, as well as physical therapy.
Although osteoarthritis was long believed to be caused by the “wear and tear” of joints over time, scientists now view it as a disease of the joint. Here are some of the factors that contribute to the development of OA:
Causes of Osteoarthritis
- Genes: Various genetic traits can make a person more likely to develop OA. One possibility is a rare defect in the body’s production of collagen, the protein that makes up cartilage. This abnormality can cause osteoarthritis to occur as early as age 20. Other inherited traits may result in slight defects in the way the bones fit together so that cartilage wears away faster than usual. Researchers have found that a gene called FAAH, previously linked to increased pain sensitivity, is higher in people with knee OA than in people who don’t have the disease.
- Weight: Being overweight puts additional pressure on hips and knees. Many years of carrying extra pounds can cause the cartilage that cushions joints to break down faster. Research has shown there is a link between being overweight and having an increased risk of osteoarthritis in the hands. These studies suggest that excess fat tissue produces inflammatory chemicals (cytokines) that can damage the joints.
- Injury and overuse: Repetitive movements or injuries to joints (such as a fracture, surgery or ligament tears) can lead to osteoarthritis. Some athletes, for example, repeatedly damage joints, tendons and ligaments, which can speed cartilage breakdown. Certain careers that require standing for long periods of time, repetitive bending, heavy lifting or other movements can also make cartilage wear away more quickly. An imbalance or weakness of the muscles supporting a joint can also lead to altered movement and eventual cartilage breakdown in joints.
- Others: Several other factors may contribute to osteoarthritis. These factors include bone and joint disorders like rheumatoid arthritis, certain metabolic disorders such as hemochromatosis, which causes the body to absorb too much iron, or acromegaly, which causes the body to make too much growth hormone.
Osteoarthritis Diagnosis
The information needed to help diagnose osteoarthritis includes:
- Description of the symptoms
- Details about when and how the pain or other symptoms began
- Details about other medical problems that exist
- Location of the pain, stiffness or other symptoms
- How the symptoms affect daily activities
- List of current medications
- Physical Examination
During the exam, the doctor will examine the joints and test their range of motion (how well each joint moves through its full range). He will be looking for areas that are tender, painful or swollen as well as signs of joint damage. The doctor will examine the position and alignment of the neck and spine.
Diagnostic Tests
A diagnosis of osteoarthritis may be suspected after a medical history and physical examination is done. Blood tests are usually not helpful in making a diagnosis. However, the following tests may help confirm it:
- Joint aspiration. The doctor will numb the affected area and insert a needle into the joint to withdraw fluid. The fluid will be examined for evidence of crystals or joint deterioration. This test can help rule out other medical conditions or other forms of arthritis.
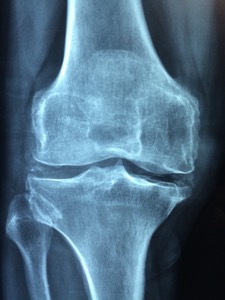
- X-ray. X-rays can show damage and other changes related to osteoarthritis to confirm the diagnosis.
- MRI. Magnetic resonance imaging (MRI) does not use radiation. It is more expensive than X-rays, but will provide a view that offers better images of cartilage and other structures to detect early abnormalities typical of osteoarthritis.
Getting Osteoarthritis Disability Benefits under a Long Term Disability Insurance Policy
We frequently review claims for osteoarthritis disability benefits that were denied by either private or employer-sponsored LTD insurance carriers.
The insurance company decides whether a claimant is disabled. They also require specific proof of disability according to the language in the policy, which is often complex and subject to multiple interpretations.
It is also quite common for insurance companies to provide claimants with short-term disability benefits for osteoarthritis, yet deny long term disability benefits.
Just because the insurance company says your claim is not valid, does not make it fact. Do not give up. Contact our firm today: we are capable, prepared and well qualified to represent you.
Contact Us Today
If your claim for long term disability insurance benefits for Osteoarhritis was denied, you need an experienced attorney to get you the benefits you deserve. Call Mehr Fairbanks Trial Lawyers without delay, for a free evaluation of your claim: 800-249-3731.
We represent disability insurance claimants all over the United States and deal routinely with the “big deniers” of group and individual LTD insurance.
(2018). Osteoarthritis. Retrieved from www.arthritis.org.
 Kentucky ERISA Disability & Life Insurance Claim Lawyers
Kentucky ERISA Disability & Life Insurance Claim Lawyers

